- NHS Continuing Healthcare Delivery Model
- Screening Process
- Full Assessment
- Verification & Decision MAking
- Review Process
- Scroll right to begin the process map
- Proportionate Screening Using Checklist
- When to complete a Checklist
- When not to complete a Checklist
- It is clear to practitioners working in the health and care system that there is no need for NHS Continuing Healthcare at this point in time. Where appropriate/relevant this decision and its reasons should be recorded. If there is doubt between practitioners, the Checklist should be undertaken.
- The individual has short-term health care needs or is recovering from a temporary condition and has not yet reached their optimum potential (although if there is doubt between practitioners about the short-term nature of the needs it may be necessary to complete the Checklist). See paragraphs 101-108 of the National Framework for how NHS Continuing Healthcare may interact with hospital discharge.
- It has been agreed by the ICB that the individual should be referred directly for full assessment of eligibility for NHS Continuing Healthcare.
- The individual has a rapidly deteriorating condition and may be entering a terminal phase – in these situations the Fast Track Pathway Tool should be used instead of the Checklist.
- An individual is receiving services under Section 117 of the Mental Health Act that are meeting all their assessed needs.
- It has previously been decided that the individual is not eligible for NHS Continuing Healthcare and it is clear that there has been no change in needs.
- What if the individual is in hospital?
Proportionate Screening Using Checklist
ICBs, along with their LA partners, should agree pro-active systems to ensure that screening arrangements are effective across all settings and for all adult client groups and should have in place agreed protocols that include arrangements for proportionate and timely use of the Checklist in accordance with the Framework requirements. This should include when it is not necessary or appropriate to screen for NHS Continuing Healthcare.
LAs and ICBs should work together to ensure that the decision whetherto Checklist, and the completion of Checklists, are undertaken by practitioners with the relevant skills and training.
The decision to undertake CHC screening should be based on the needs and situation of the individual ratherthan on administrative or organisational requirements (e.g.,screening purely because the individual’s case is being considered by an LA funding panel).
Health and Social Care agencies are responsible for ensuring that any Checklists completed by their staff are of good quality and accurately reflect the individual’s needs.
ICBs should not impose disproportionate quality assurance mechanisms for Checklists which result in a barrier to, or delay in, individuals being referred for CHC assessment. Positive Checklists should be acted upon as soon as possible unless critical information is missing, in which case the missing information should be obtained without delay.
Where poor practice regarding screening is identified in a team/environment then targeted intervention (for example bespoke training) should be provided in order to address the issues.
ICBs and system partners should agree an escalation process if cases are being checklisted inappropriately or are being denied a Checklist inappropriately. This could form part of the locally agreed dispute resolution process/policy.
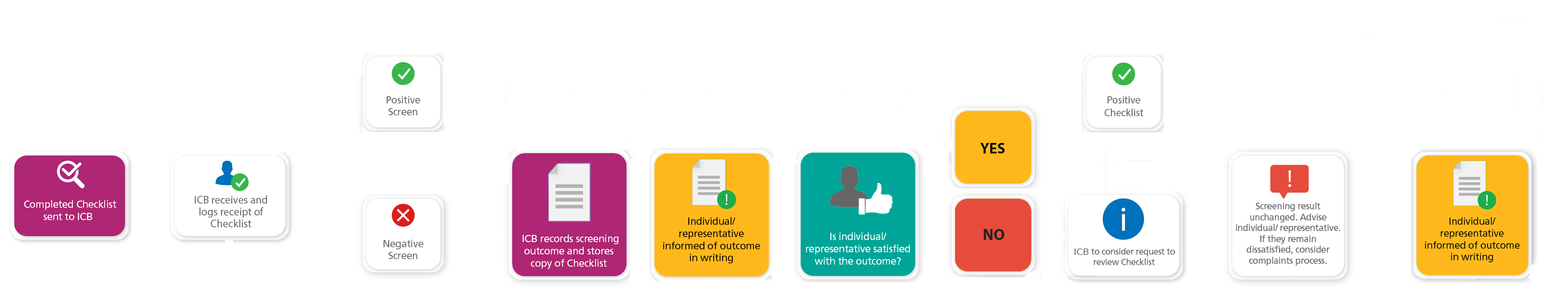
Arrangements must be in place to inform individuals and/or their representatives of the outcome of the Checklist (whether positive or negative) in writing. There should be agreement between health and social care agencies as to how this requirement will be met, bearing in mind that Checklists are completed by a wide range of practitioners acrossdifferent organisations. Joint Statements –Proportionate Screening Page 3 of 3.
Health and social care agencies should agree arrangements to ensure that the ICBreceives completed Checklists as soon as possible after completion andthat it keeps a recordof the outcome of all Checklists completed, both positive and negative.
When to complete a Checklist
“Where there may be need for NHS Continuing Healthcare, the Checklist should normally be completed.
There will be many situations where it is not necessary to complete the Checklist. See paragraph 121 of the National Framework and page 9 below.
Screening and assessment of eligibility for NHS Continuing Healthcare should be at the right time and location for the individual and when the individual’s ongoing needs are clearer. This may be in a variety of settings, although the full assessment of eligibility should normally take place when the individual is in a community setting, preferably their own home. The core underlying principle is that individuals should be supported to access and follow the process that is most suitable for their current and ongoing needs. This will help practitioners to correctly identify individuals who require a full assessment of eligibility for NHS Continuing Healthcare.
To understand how NHS Continuing Healthcare interacts with hospital discharge, please refer to paragraphs 101-108 of the National Framework.”
NHS Continuing Healthcare Checklist Guidance: Paragraphs 5-8
A positive Checklist means that the individual requires a full assessment of eligibility for NHS Continuing Healthcare. It does not necessarily mean the individual is eligible for NHS Continuing Healthcare
National Framework (2022), Paragraph 134.
When not to complete a Checklist
There will be many situations where it is not necessary to complete the Checklist.
Practitioners should review the statements below on when it may not be appropriate to screen for NHS Continuing Healthcare before they start the process of completing the Checklist.
The situations where it is not necessary to complete the Checklist include:
NHS Continuing Healthcare Checklist Tool Page 9
Patients in Hospital
For patients who are in hospital, the process that is most suitable for their current and ongoing needs should be followed. For guidance on proportionate and timely screening, see paragraphs 88-91 of the National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care (revised 2022). For more detail on how NHS Continuing Healthcare (CHC) interacts with hospital discharge, see paragraphs 106-117 of the National Framework 2022, remembering that very few patients should be assessed for CHC in an acute setting. For further information, please refer to “Understanding how Hospital Discharge Interacts with Continuing Healthcare”.
Paragraph 109 of the National Framework 2022 states ‘In the majority of cases, it is preferable for eligibility for NHS Continuing Healthcare to be considered after discharge from hospital when the person’s ongoing needs should be clearer. The aim in most cases will be for the individual to return to the place from which they were admitted to hospital, preferably their own home. It should always be borne in mind that an assessment of eligibility for NHS Continuing Healthcare that takes place in an acute hospital might not accurately reflect an individual’s longer-term needs. This could be because, with appropriate support, the individual has the potential to recover further in the near future. It could also be because it is difficult to make an accurate assessment of an individual’s needs whilst they are in an acute services environment.’
National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care (revised 2022)- Icon
How hospital
discharge interacts
with CHC - Screening Guidance
Screening
Guidance
Finding out about CHC
Finding out about the Checklist
Understanding the purpose and process of CHC

An appropriately trained professional is appointed to carry out a Checklist and explain the screening process to the individual
- Who can complete a checklist
Who can complete
a checklist
- Capacity - 5 Principles
- A person must be assumed to have capacity unless it is established that they lack capacity.
- A person is not to be treated as unable to make a decision unless all practicable steps to help them to do so have been taken without success.
- A person is not to be treated as unable to make a decision merely because they make an unwise decision.
- An act done, or decision made, under this Act for or on behalf of a person who lacks capacity must be done, or made, in their best interests.
- Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person’s rights and freedom of action.
Consent
It must be remembered that consent is not required to process personal data for CHC purposes – this can be carried out using the public task/official authority and provision of healthcare processing conditions. Using consent as the basis for processing personal data will mean that you give the patient the right to withdraw that consent at any time and in any form (verbal or written). If they do this, you cannot switch to a different processing condition to carry on providing CHC assessment and care and circumvent the wishes of the patient.
However, you will still need to obtain consent to satisfy the Common Law Duty of Confidence, and it is important to be clear that you are obtaining consent for Confidentiality and not processing. You will still need to inform the patient about the use if their information, so they can give their consent based on what they expect to happen.
Mental Capacity - 5 principles
If there is a concern that the individual may not have capacity to give consent to a physical intervention/examination as part of the NHS Continuing Healthcare assessment process or the sharing of personal data with family, friends, advocates, and/or other representatives, this should be determined in accordance with the Mental Capacity Act 2005 and the associated code of practice. ICBs should be particularly aware of the five principles of the Act:
It is important to be aware that just because an individual may have difficulty in expressing their views or understanding some information, this does not in itself mean that they lack capacity to make the decision in question. Appropriate support and adjustments, for example, using alternative methods of communication, should be made available to the person in compliance with the Mental Capacity Act 2005, and with disability discrimination legislation. (National Framework 2022, Paragraphs 86 –87)
References
1. Mental Capacity Act Code of Practice 2005
2. National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care (revised 2022)
3. Section 1(3) and Section 3(2) Mental Capacity Act 2005
4. Equality Act 2010
- Consent Form
Consent
form - Principles of Consent
Principles
of Consent - Best interest decision guidance
Best interest
decision
guidance
Scheduling the DST meeting – Ensuring appropriate attendance
Communications and language
- 28 Day Clock Starts
28 Day Clock Starts